Tumors can be effectively treated for multidrug resistance using a highly efficient nanosystem with multifunctional capabilities

P-glycoprotein (P-gp/ABCB1) is a typical type of multiple drug resistance (MDR) transport protein that can recognize and promote the drug efflux of tumor cells, severely limiting the efficacy of anti-tumor drugs.
BAY-1082439, a specific inhibitor against phosphatidylinositol-3-kinase (PI3K) 110α and 110β subunits, can reverse P-gp-mediated MDR by down-regulating P-gp expression. However, BAY-1082439 has shortcomings such as poor water solubility, short half-life, and high clearance rate in vivo.
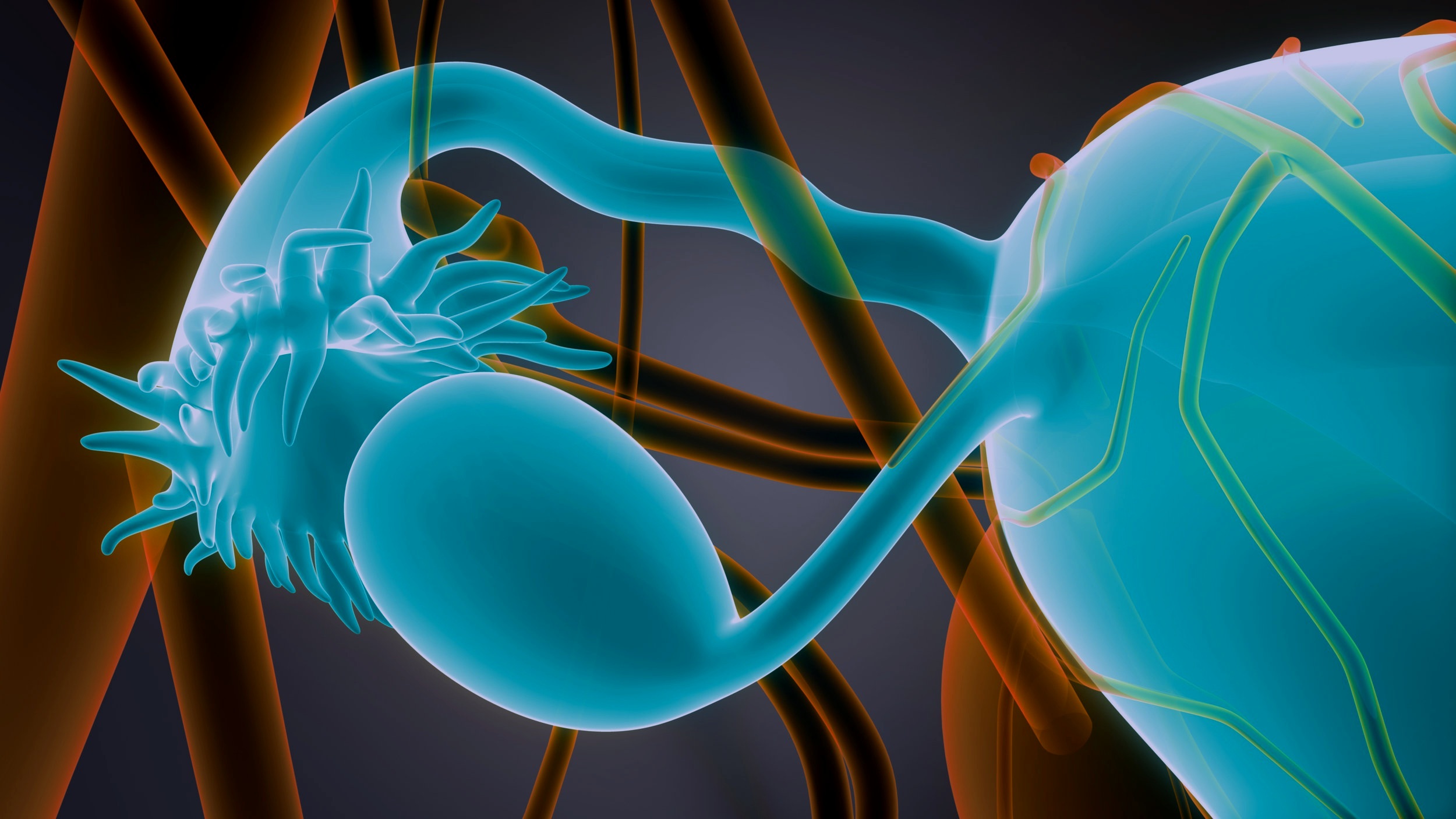
A research group led by Prof. Chen Zhuo from the Fujian Institute of Research on the Structure of Matter, Chinese Academy of Sciences, has established a tumor targeting drug delivery nano-system PBDF [P: poly(L-lactide-co-glycolide)-Thiol (PLGA-SH); B: BAY-1082439; D: doxorubicin (DOX); F: Folic acid-polyethylene glycol-Thiol (FA-PEG-SH)].
It comprises doxorubicin (DOX) and BAY-1082439 respectively encapsulated by biodegradable PLGA-SH nanoparticles (NPs) that are grafted to gold nanorods (Au NRs) modified with FA-PEG-SH, which can enhance the efficacy to reverse P-gp mediated MDR and to target tumor cells, and finally the efficiency to inhibit MDR tumors overexpressing P-gp. The study was published in Cancer Letters.
"Compared with free DOX combined with BAY-1082439, PBDF NPs significantly enhanced the uptake of DOX, improved the activity of reversing MDR, inhibited cell proliferation, and induced S-phase arrest and apoptosis of KB-C2 cells," said Prof. Chen.
The in vivo animal experiments further confirmed that PBDF NPs enhanced the anti-tumor ability of DOX and inhibited the development of KB-C2 tumors.
Besides, PBDF NPs inhibited the metastasis of KB-C2 cells in the liver and/or the lung of nude mice but had no obvious toxic effect on normal cells.
This study develops an achievable and applicable targeted therapy strategy for MDR tumors with high biocompatibility and the potential to inhibit MDR tumor progression and tumor metastasis.