Nanomedicine researchers target disease at the molecular level

Adam Hall, Ph.D., isn't kidding when he says the research he does is on a very small scale. But he is understating things more than just a little.
Hall works in nanomedicine, a relatively new but rapidly developing branch of nanotechnology -- the study, development and application of materials between 1 and 100 nanometers in size -- that is devoted to the diagnosis and treatment of disease.
What exactly is a nanometer?
It's exactly one-billionth of a meter. A meter is 3.28 feet, or 39.37 inches, so a nanometer is 0.0000003937 of an inch. That means there are 25,400,000 nanometers in an inch.
In perhaps more understandable terms, a sheet of paper is about 100,000 nanometers thick and a typical human hair is roughly 80,000 nanometers wide. A strand of human DNA, conversely, is around 2.5 nanometers in diameter. Which is way past very small.
"Technology, in the broadest sense, has evolved to the point where we can look at things closer and closer and effectively work with smaller and smaller amounts of stuff," said Hall, an assistant professor of biomedical engineering at Wake Forest School of Medicine, which is part of Wake Forest Baptist Medical Center.
"Ultimately, for cancer and other diseases that we worry about, the root causes are molecules. People may talk about malfunctioning cells, but what happens inside those cells to make them dangerous happens at the molecular level. That's at the nanoscale, and that's why we're working there."
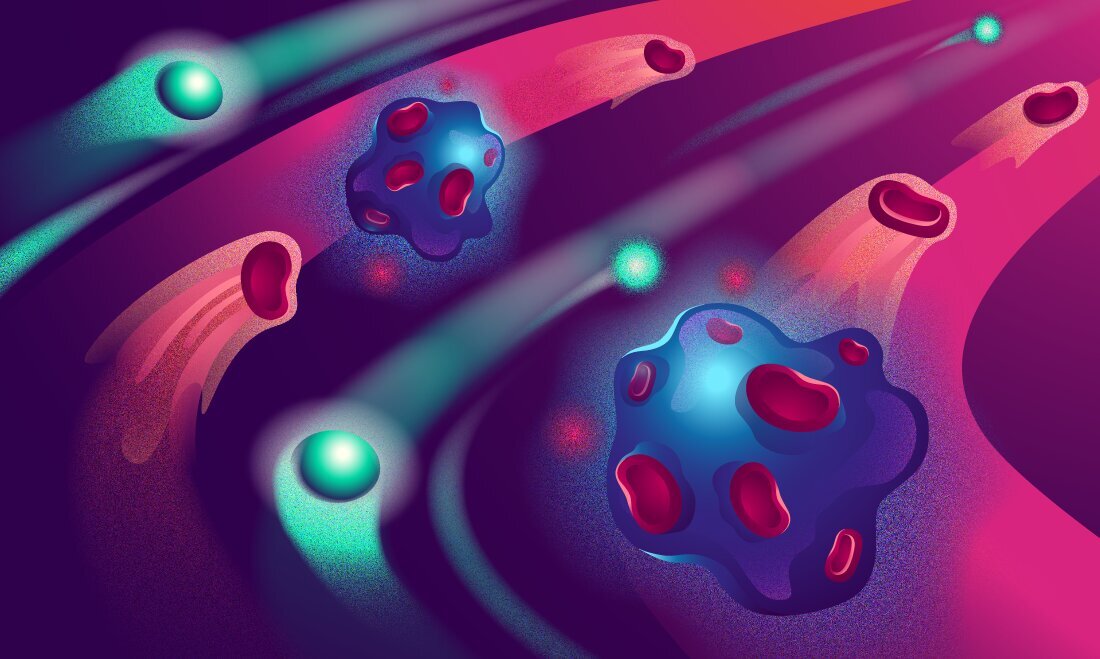
Hall's research is on the diagnostic side of nanomedicine and is centered on nanopores -- nanoscopic holes in synthetic membranes through which individual molecules can be threaded. As the molecules pass through, a nanopore in an electrically charged membrane can "read" information about them by measuring changes in the flow of current.
Using a nanopore device with a pore less than 10 nanometers wide, Hall and colleagues have developed a methodology capable of detecting and counting specific DNA and RNA sequences, including those of microRNA, a class of nucleic acid no more than 10 nanometers long and a single nanometer wide that can be a biomarker of disease.
"MicroRNAs are very tiny pieces of nucleic acid that carry genetic messages and are floating through your bloodstream all the time," Hall explained. "But if the cells producing them are diseased, whether from cancer or something else, the RNAs they release can act like messages in bottles, indicating the presence or progression of the disease."
Hall first successfully demonstrated his methodology with a microRNA known to be an indicator of lung cancer, and he is confident that the fast, noninvasive diagnostic process, potentially requiring only a tiny blood sample, will work just as efficiently in detecting the presence -- or absence -- of other diseases.
"It's a modular technique that can be applied to a whole bunch of different targets," he said. "As long as we know the sequence of a nucleic acid that's linked to a certain disease, we can seek out those particular molecules so only they will produce a signal that we can record when they pass through the nanopore."
Wake Forest Baptist recently a $75,000 grant from the North Carolina Biotechnology Center in support of Hall's efforts using the nanopore device to detect viruses responsible for infectious diseases. But Hall has no intention of stopping there. He believes his nanopore technique can also be adapted to recognize pathogenic bacteria and key genomic DNA sequences, or detect multiple distinct sequence biomarkers in tissue and biological fluids. Eventually, he hopes to develop the technology into a commercial device that will fit in the palm of a hand.
In a different Wake Forest School of Medicine lab, Nicole Levi-Polyachenko, Ph.D., an associate professor of plastic and reconstructive surgery, is working in a different area of nanomedicine, specifically with a nanoparticle created to both locate and destroy diseased cells.
"What it does is detect and treat," she said. "But I like to think of it as trap and zap."
The nanoparticle, which is less than 100 nanometers in diameter, contains two semiconducting polymers -- one fluorescent, one heat-generating -- originally designed for solar energy applications by Wake Forest University's Center for Nanotechnology and Molecular Materials that have been modified by Levi-Polyachenko for medical use.
These two polymers are "wrapped" in a coating that directs the nanoparticle to attach itself to a specific type of cell. The fluorescent polymer can identify the targeted cells by lighting up when exposed to colored light, and the thermal polymer can destroy those cells by heating up upon exposure to infrared light.
"There are limitations with some imaging techniques so physicians often have to rely on sight and feel to determine what tissue needs to be removed, and it can be hard to tell what's diseased and what's not," Levi-Polyachenko said. "What we want is a way of detection that's extremely precise, and with the nanoparticle what's diseased lights up and what isn't doesn't.
"As for treatment, the goal is to destroy the diseased tissue while saving as much healthy tissue as possible. Surgery may involve the removal of some healthy tissue, and treatments like chemotherapy affect both diseased and non-diseased cells. But these nanoparticles only attach to the targeted cells and when they're heated up, they kill just those cells and they kill them for good. There's no collateral damage."
Working in animal model, Levi-Polyachenko's research team has successfully demonstrated the nanoparticle's ability to locate and destroy colorectal cancer cells. Current research is targeting breast cancer cells and harmful bacteria. If all continues to go well, Levi-Polyachenko said, the two-polymer nanoparticle could be approved for use in humans within 10 years.
"We're really not all that far off," she said.
Source: Wake Forest Baptist Medical Center.